Regardless of the reason, losing a limb is never easy. Both mentally and physically, amputation can negatively affect a person and inevitably changes their life as well as the lives of their loved ones. While it may not be a cakewalk, life after amputation is simply a matter of finding a new routine — a new normal.
For new amputees, the whole process can seem intimidating, but it is always important to remember that no one goes through an amputation alone. There are lots of resources and organizations available to help with everything from pre-surgery consultations to programs for life-long peer support.
A good way to calm fears is to learn as much as you can about the thing that scares you, so we have created this guide to help new amputees understand how to deal with amputation by explaining what happens through the different stages of this life-changing surgery.
What to Expect Immediately After Amputation
When you have decided that amputation is necessary, you will want to understand what to expect before the surgery and after the surgery. It can also be helpful to understand what happens during the surgery as well, even though you will be asleep for it.

Before the Surgery
You will likely have a rehabilitation team that will include surgeons, nurses, physical therapists, occupational therapists and social workers. This team will guide you through the rehabilitation plan, which they will create with your input. They may also provide you with some exercises or stretches to do that will help the wound heal more quickly.
If you have not already chosen a prosthetist, choosing one before the surgery is recommended. You will be working with the prosthetist very closely following your surgery and, hopefully, you will develop a long-lasting relationship with them. They will help you a lot during the first year after your surgery as you learn how to adapt to your prosthetic limb, and they may even be a part of your rehabilitation team.
The rehabilitation team is full of knowledgeable professionals, so they are the best people to turn to with any questions or concerns you may have about the surgery or rehabilitation. It is essential you are actively involved in your rehabilitation. Your rehabilitation team may also be able to direct you to others who have experienced an amputation so you can get a first-hand account from someone who has been where you are.
Emotionally, it is very normal to be scared, shocked, angry or overwhelmed. There is no wrong way to act in this scenario.
During the Surgery
When amputating a limb, the surgeon will also remove any damaged tissue, leaving as much healthy tissue as possible. They may also remove any pieces of crushed bone and then smooth out any uneven areas of the remaining bone. Smoothing out the bone will allow tissue and muscles to adequately cover it, and the surgeon may even stitch the muscles to the bone to help strengthen the area.
After the Surgery
The first day after the surgery is often the hardest as you process that what was previously just theoretical is now a reality. The wound will be dressed in bandages and compressions socks, and possibly also elevated or put in a stint, to help reduce swelling, which is very likely after surgery. Ensuring swelling stays down and the residual limb — the part of the limb still attached to the body — shrinks is a priority during this time. Proper healing will make it easier to fit a prosthetic limb later on.
The nurses and physiotherapists will be the professionals you see the most immediately after the surgery since you will likely be receiving oxygen from a machine and getting fluids from an IV drip. You may also have a urinary catheter attached to avoid you needing to get up to use the bathroom since the wound will need to be kept stable.
Rehabilitation will begin within a few days, but it will mostly be very simple and gentle stretching exercises to help you maintain the range of motion in all your other limbs. The physiotherapist will likely also guide you through some exercises to prevent blood clots from forming.
As it was before surgery, it is still important that you communicate any discomfort or concerns to your rehabilitation team. This includes any pressure points in the bandages or any pain in the residual limb.
The wound itself will take anywhere from four to eight weeks to heal fully, but you will likely only remain in the hospital for up to 14 days. The lengthy stay in the hospital is to allow doctors to monitor your healing and keep an eye on any conditions that may interfere with proper healing, such as diabetes or hardening arteries. They will also prescribe painkillers and other medications to prevent infections.

The Healing Process
What is the recovery after amputation like? Well, the short answer is that it’s long and can last years. The long answer is that amputation is not just the physical loss of a limb — it is also the readjustment of a person’s very way of living and requires relearning how to do many things that were once second nature.
The healing process begins with three main components:
- Physical therapy and rehabilitation
- Managing the risk of complications
- Gaining mobility and independence
If you plan on getting a prosthesis, it may be months before you are fitted for your artificial limb, which makes physical therapy one of the most important parts of your recovery.
Physical Therapy and Rehabilitation
A part of rehabilitation is strengthening the muscles in your remaining limbs, and another part is helping you work towards independence. In the beginning, physical therapy will be difficult and frustrating, but just remember that it is the first step to getting back on your feet — figuratively and maybe even literally.
Your therapist will not expect you to strain yourself on the first day. Instead, you will start with gentle movements that will gradually become more active and strenuous. You will learn how to exercise the muscles in the other parts of your body, which will be used more than they were before the surgery.
When you have been discharged from the hospital, an occupational therapist may visit your home to see if it needs any adjustments to accommodate your change in mobility. For example, you may need to have a ramp installed.
You will continue to see more of the hospital in the weeks after since you will need to return to change your bandages and let the doctor see how your wound is healing and how you are adjusting to your new life at home. You may end up returning to have sutures removed, after which you will start wearing a compression sock on your residual limb to help it shrink even more. The shrinkage is necessary because it molds the stump, which helps it fit the prosthesis easily and more comfortably.
The stump will be a healing wound and, like any other healing wound, it needs to have adequate care to speed up healing and prevent infections. It is best to avoid submerging the stump in water, such as if you take a bath.
Managing the Risk of Complications
Like with any major surgery, there are risks of complications involved with amputations. These can include:
- Heart problems, including heart attacks
- Deep vein thrombosis, which is a fancy way of saying a blood clot that forms in the veins of your legs
- A slowdown of healing, potentially due to infection
- Pneumonia
- Phantom limb symptom, which is common for amputees
The need for further surgery is also a potential, especially if there is pain, such as from nerves that have thickened, or if more tissue needs to be removed.
Gaining Mobility and Independence
Once you are discharged from the hospital, you will need to learn how to do everyday activities with your revised body. Your rehabilitation team will be able to provide you with the appropriate mobility devices as well as living aids to help you ease back into your everyday life.
These devices will be crucial as you get used to embarking on your usual household tasks and activities with your residual limb, and they are designed to help amputees become more independent.
Long-Term Care and the Road to Recovery
When it comes to the long term, there are two parts of the recovery process:
- Physical recovery
- Emotional recovery
Both physical and emotional recovery is something you will be doing from the time of your surgery on, but while physical recovery likely has an end date, emotional recovery can be ongoing.

Physical Recovery
Physical recovery includes physiotherapy, which you will likely have to do three to five times a week. As we mentioned before, physical therapy may seem like a chore, but it is one of the most critical parts of recovery since it helps the body adapt to its new normal. Physiotherapy exercises are designed to help you learn how to redistribute your weight and balance with missing lower limbs or exercise your other limbs, which will be used more often, without injuring them.
These exercises are designed to help a person return to their regular routine by relearning how to do everyday activities. The exercises help you strengthen muscles to be able to better control limbs. Similarly, rehabilitation will also help you learn to live without the limb that has been amputated, which will decrease the chances of developing phantom limb syndrome.
Learning to care for the existing limbs — especially if the amputation was a result of a disease, like diabetes — and actively taking better care of the existing limbs to keep them from coming to harm are also necessary lessons during physical recovery.
Once you are fit for a prosthetic limb, you will learn how to move with an artificial limb and get used to living life with it. You will also learn how to care for your prosthesis.

Emotional Recovery
There are no wrong feelings when it comes to amputation, which is why emotional recovery is as important as physical recovery. The psychological impact of an amputation can run the gamut of emotions, with grief and bereavement being some of the most common emotions. The grief is sometimes strong enough to be likened to the death of a loved one.
Three key reasons an amputation can have such a strong effect on a person’s life are:
- Getting used to the lack of feeling and sensation in the amputated limb.
- Getting used to the lack of function of the amputated limb.
- Adapting to a new sense of body image.
How other people view your body may also have changed, and coping with that is another significant factor.
Negative thoughts are extremely common and very much normal during this time, and they can be as mild as temporary frustration or sadness to suicidal ideation. Your rehabilitation team should be on top of these thoughts and, once you are discharged from the hospital, you may be directed to counseling or therapy to help you deal with these feelings constructively.
Feelings of negativity are more likely to be present if the amputation was done suddenly — such as after an accident or similar trauma. Without the opportunity to get used to the reality of what amputation means, it can be incredibly difficult to cope with it in the aftermath.
Sometimes, there is an inability or unwillingness to accept the amputation as reality. Some people may refuse to accept that they will need to alter their lifestyles because of the amputation and may refuse help. Other times, post-traumatic stress disorder is possible, especially when the amputation is the result of severe trauma.
1. Phantom Limb Syndrome
Possible the most common psychological side effect of amputation is phantom limb syndrome, which is when you believe you can feel the limb that has been amputated. While most amputees feel like they can sense the amputated limb, not all of them feel pain in it. The phantom sensation comes from the spinal cord and the brain.
Phantom pain, on the other hand, is still a bit of a mystery. Theories about the cause of phantom limb pain suggest it has something to do with the brain’s reorganization after amputation. When a limb is amputated, the communication between the neurons in certain nerves and the brain is broken. Eventually, those neurons are reactivated and begin communicating with the brain again by responding to input from the nerves that remain. Sometimes, putting pressure on the residual limb is the trigger for this communication, causing the amputee to feel phantom pain.
Both phantom pain and phantom sensation are common occurrences and tend to affect older amputees. It can develop immediately after amputation or even weeks, months or years later. Stress, anxiety and fear are all potential triggers for phantom pain, and the pain itself can range from sensations of aching and cramping to burning or shock.
Many people find that they no longer experience phantom pain once they have a prosthesis, but some home remedies can help alleviate phantom pain, including:
- Wrapping the residual limb in a warm towel or heating pad.
- Applying a cold cream or ice pack to the residual limb.
- Massaging the residual limb and mentally exercising the missing limb.
- Changing positions by standing up or moving around.
- If you have a prosthesis, putting it on and going for a walk sometimes helps for lower-body amputations.
- Tightening and slowly releasing the muscles of the residual limb.
Prosthetics — Fitting and Care
Approximately two or three weeks after the surgery, you will be fit for a prosthetic limb. The wound has to have healed well enough to begin the fitting — which involves making a cast of the residual limb. It can take upwards of six weeks if the wound is not healed properly or is taking longer to heal.
A prosthesis generally has seven parts:
- A gel cushion interface to protect the skin on the residual limb and adjust the pressure
- A suspension system to connect the artificial limb to the body
- The socket, which is the part that attaches on to the residual limb
- Joints and appendage
- A system of endoskeletal connections to link the joints and appendages while providing adjustability
- A soft, foamy material that mimics muscles and also protects the endoskeletal connections
- Synthetic skin that is applied all over the anatomic shape to mimic human skin
Getting Fitted for Your Prosthesis
Once it is healed, the prosthetist will take a mold of your residual limb using plaster or 3D imaging, which be then be altered to better fit the residual limb. A socket will be created to fit the stump comfortably, and a temporary, diagnostic prosthesis will be attached to it. The socket fit is crucial since that part will be right up against the stump and needs to be extremely comfortable for both comfort and safety.
The temporary limb is used to make adjustments based on your individual needs. The temporary limb helps test various combinations of components to adjust comfort, stability, functions and efficiency. Since each prosthetic limb is unique to the person donning it, many adjustments and trials need to be made before the final product is ready. Generally, you will need to visit your prosthetist between seven and 18 times, and there will be about 16 temporary or sample pieces created before the final one.
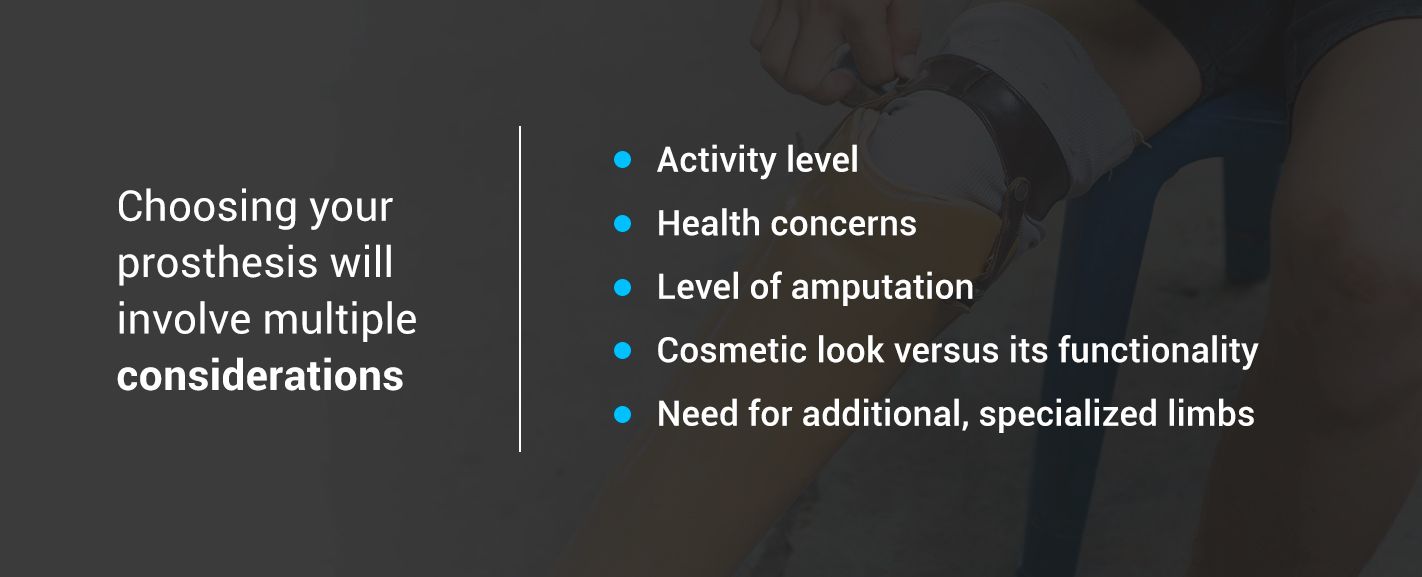
Choosing your prosthesis will involve multiple considerations, including:
- Activity level
- Health concerns
- Level of amputation
- Cosmetic look versus its functionality
- Need for additional, specialized limbs
A higher amputation may require a prosthesis with more parts, or an athlete may want an extra prosthesis specifically for sports. For example, a bicyclist may need alterations to an arm prosthesis and bike to ride safely.
It is normal to feel some pain when you first don your new prosthesis since your body will need to get used to the new addition. Still, it is always a good idea to describe any and all pain or discomfort — like pinching or poking, for example — to the prosthetist, just in case the artificial limb needs to be adjusted in any way.

Caring for Your Prosthesis
The prosthetist is a professional, and they know their business, which is why it is best to listen to their instructions and advice. Just as important is asking your own questions and getting clarification on anything — no matter how silly it may seem to you. There will likely be a lot of information coming your way, and it can be very overwhelming. A good idea is to take notes during your meetings with the prosthetist so you can refer back to them later. Similarly, jot down any questions you may have between appointments so you remember to bring them up with the prosthetist.
Some general tips can be applied to all new amputees:
- Do not overdo it. It may be tempting to don your prosthesis and return to your life before the amputation, but remember that your entire body is healing from the amputation, so it needs plenty of time to rest and adapt. The prosthetist will provide you with a wearing schedule, so make sure to follow it to avoid any complications.
- Do use assistive devices. Assistive devices like canes can be an asset in the early weeks of wearing a lower prosthesis. The human body naturally will want to put all pressure on the remaining limbs, but you need to learn how to balance your weight evenly between your prosthesis and your remaining limb. Using an assistive device will help you to gradually shift weight onto the prosthesis.
- Do not ignore changes in your prosthesis. However well you care for your prosthesis, it could break. If you hear any clicking, creaking or squeaking coming from your prosthesis when you put it on, point it out to the prosthetist. Remember, your prosthesis is custom-made for you, so any changes can be detrimental to your progress.
- Do work at being active without prosthesis. You need to build up the stamina for wearing the prosthesis so you can return to a highly independent life.
- Do not ignore the residual limb. Examine your stump every day and report any signs of redness, blisters or pain to the prosthetist. Make sure to clean your prosthesis using anti-bacterial soap and warm water after every time you remove it. Later, make sure it is completely dry before donning the prosthesis.
The stump size will fluctuate for a while before settling on its final size. The goal is to get it as small as it can be, so wearing shrinker socks is crucial whenever you are not wearing the artificial limb. As their name suggests, shrinker socks will help mold the stump into a smaller, rounder shape. Of course, as the stump changes sizes and shapes, the socket will need to be adjusted accordingly to ensure the prosthesis is still comfortable.
If you are getting a prosthetic leg, you need to be aware of the heel height. The artificial limb is made for a specific heel height — likely to match your remaining limb’s heel height in your most comfortable pair of shoes — so adjusting the heel height of your remaining limb can put your body off-kilter, which can then lead to more complications down the road. Always check with your prosthetist before you change your heel height.
Being crammed into a socket all day will inevitably make your residual limb perspire. Cleanliness is particularly crucial. The buildup of sweat and dirt can lead to various skin issues, thanks to the bacteria that will form. Additionally, your residual limb is likely to develop an odor. Aside from cleaning your stump every day, you can also try sprinkling some baking soda on the stump before wearing your prosthesis to help reduce the amount of sweat. Similarly, you can also apply some over-the-counter antiperspirant to the stump before donning the prosthesis. And while you are cleaning up, remember to clean up the socket as well.
The good news is the more you wear your prosthesis, the less you will perspire as your body gets used to its new normal. Still, keep checking on your residual limb for any injuries — like blisters or tender areas —as well as your remaining limb, especially if the reason for your amputation was due to health issues, like diabetes.
Prosthetic Training: What Is It and Why Does It Matter?
As with anything else in life, practice makes perfect, and donning your new prosthesis is no different. You may feel like that wearing a prosthesis will be exactly like having your amputated limb back, and while science and technology have come far enough for that to be closer to true, the human body still requires some level of training to adapt.
What is natural is how the human body responds to something like an amputation. When a limb is lost, the body will automatically put more of the burden on the remaining limbs to make up for the lost one. Prosthetic training is getting the body to unlearn what comes naturally and relearn how to function as if it was still working with all original limbs.
For example, if you have had a leg amputated, your body’s natural reaction will be to shift the burden on to the remaining leg. But with a prosthesis, your body needs to learn how to evenly distribute the weight between the artificial and remaining leg. Continuing to place most of your weight on your remaining leg instead of on the prosthesis can cause various health problems down the line — and is likely to be uncomfortable.
Retraining Your Body
Regardless of which limb has been amputated, your body will need retraining to function properly with the prosthesis.
For example, leg or foot amputations will require gait training, which teaches your body how to walk naturally again instead of limping. This is crucial since the proper way of walking helps reduce the risk of multiple injuries in the back and legs. Gait training also helps take the pressure of the residual limb, which reduces the chances of injury.
Similarly, if you had an arm or hand amputation, you will need to relearn how to do many things you previously took for granted, such as how to get dressed by yourself. An occupational therapist will likely teach you tips and tricks to living independently with an amputation — both for doing things with and without your prosthesis. Putting on shoes, cooking dinner and even driving are all things that you will need to relearn, even with a prosthesis.
The reason is that the prosthesis is unable to mimic many of the very fine motor skills that human hands are capable of. This does not mean that you cannot do things requiring fine motor skills, just that you have to learn new ways to do them. An occupational therapist will help you learn to mimic some of those fine motor skills, such as the ones needed for eating with cutlery or going up and down the stairs.
The amount of time the training takes varies from person to person and can be further complicated by the type of prosthesis being used. Each prosthesis requires specific training because no two artificial limbs are alike. You should know exactly how to use your own prosthesis so you can live a highly independent life.
Importance of Independence
The main goal of prosthetic training and occupational therapy is independence. In the past, an amputation meant the end of your former life altogether. The technology was not advanced enough to allow amputees to do things independently. Instead, they were highly dependent on others.
Today, technology and our understanding of the human body and mind have come so far that amputees no longer need to be dependent on others to live a fulfilling life. With training, living aids and ongoing support, amputees can return to their independent lives. They can participate in sports, cook, drive — whatever they want.
The effect of independence goes beyond just physical rehabilitation — it is also vital for emotional rehabilitation. Many feelings come with an amputation, and regaining independence can help you feel more like yourself. Being independent and returning to the tasks you once did without a second thought can also help you become more comfortable with your new body image and your new reality. It can boost your self-confidence and help alleviate feelings of grief and anger that often accompany an amputation.

Newfound Challenges — How Does Amputation Affect a Person’s Life?
No matter how much you prepare, you will likely still experience challenges you never considered. You may feel that an amputation limits what you can and cannot do, but those limitations are more like pushes to alter how you do things. For someone with an arm or hand amputation, relearning how to do seemingly simple tasks, like brushing your teeth, may become a challenge. Someone who has had a leg amputation will inevitably need to relearn how to walk and run.
Luckily, living aids can assist those with amputations and encourage them to live more independent lives. From tools to help chop up vegetables to handlebars to make climbing in and out of the bath easier, almost anything that a non-amputee can do, an amputee can do as well.
Bathroom activities are often the most concerning for new amputees. Even if you do not mind asking for help in the kitchen or with household chores, everyone prefers to tend to bathroom duties by themselves. As mentioned, because prostheses are unable to mimic the fine motor skills needed for certain tasks — such as holding a toothbrush to brush teeth properly — living aids help make these tasks a bit easier. You can even make some do-it-yourself living aids, like wrapping some tape, or other anti-slip devices, on a toothbrush to help the prosthesis grip it better.
Ways to Cope With an Amputation
As we mentioned, the emotional impact of an amputation can be severe and there is no wrong way to deal with your amputation. Grief, anger, depression are just some of the possible emotions you will feel — and they are all valid and very normal. The important thing is how you cope with these feelings, whatever they are.
There are healthy and unhealthy ways to cope with an amputation. For example, refusing to deal with the reality and impact of your amputation is an unhealthy way to cope. Here are some healthy ways for how to deal with amputation:
- Accept and acknowledge your feelings: Whatever the feelings are, do not ignore them — even the negative ones. Acknowledging the good and bad feelings is the first step in dealing with them. Instead of forcing yourself to always be positive, allow yourself to be sad or angry if that is how you feel — and remind yourself that you are allowed to feel that way.
- Focus on the journey: Rehabilitation from an amputation does not have a timeline. It varies for everyone and can take years. Emotional rehabilitation is often a lifelong task, so focus on the end goal is rarely helpful. Instead, learn to appreciate your progress so far and try not to obsess over how far you still have to go. Rehabilitation consists of millions of baby steps and each little step is progress worth celebrating.
- Find a purpose: Whether it is spiritual or altruistic or just for fun, find something that makes you excited to wake up in the morning. Some people like to volunteer with organizations that help amputees while others take up hobbies to master. Whatever it is, find just make sure it makes you glad to be alive and working towards recovery.
- Learn to think of yourself in a new way: Instead of focusing on what you can no longer do, try to focus on everything you can still do — and have learned to do since the amputation. Rearranging how you see yourself can boost your mental health and self-confidence and helps normalize amputees for others.
- Talk to other amputees: No matter how well-meaning your loved ones and rehabilitation team are, unless they are an amputee as well, they will not know what it is like for you. Support groups for amputees can be a space in which you can truly feel like your experience is understood because the chances are that other amputees have been through it as well. They can also provide relevant coping mechanisms non-amputees have not considered.
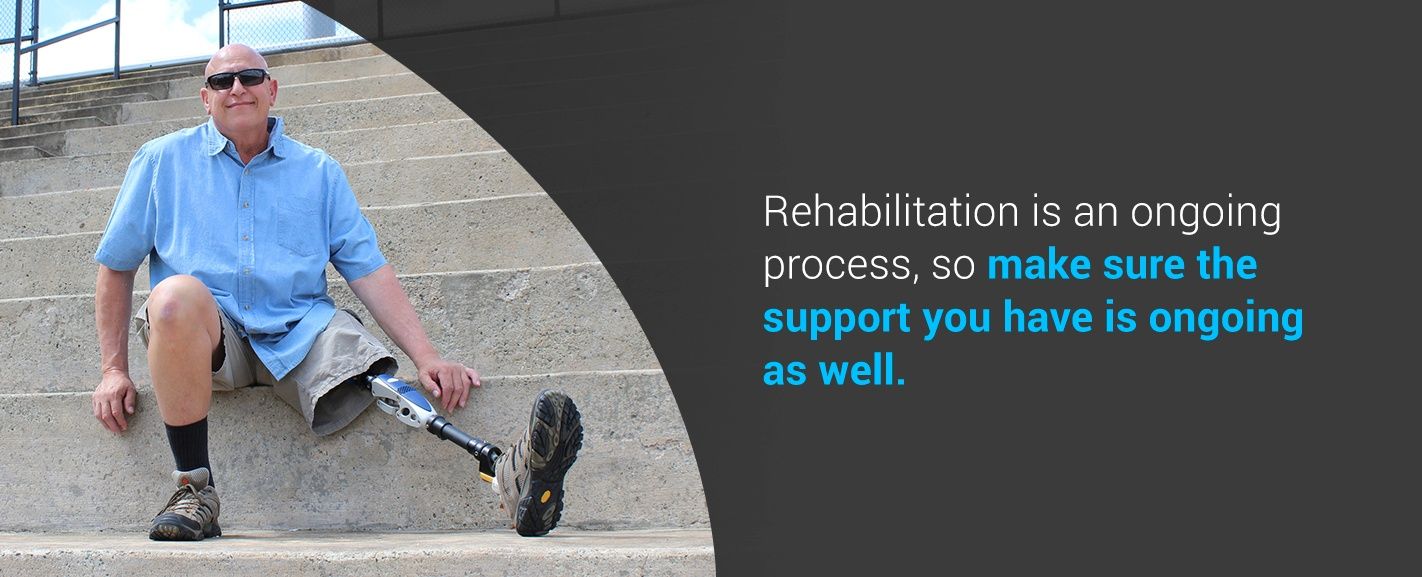
The Importance of Ongoing Support
Rehabilitation is an ongoing process, so make sure the support you have is ongoing as well. While peer support is crucial, so is the support of your rehabilitation team. Your general practitioner, physiotherapist, prosthetist and therapist are just some of the members of your ongoing support team — people you will build relationships with and see for many years following your amputation.
Ongoing support is also where your loved ones can get support — they will likely feel a level of grief and loss or even just stress due to your amputation. Providing ongoing support to you and your loved ones ensures that you never suffer.
Whether you are a brand new amputee or have been one for decades, no one is immune to needing help once in a while. Though you may need it less as you grow older, it is unlikely that a time will come when you do not need any support whatsoever.
Despite advancements in technology, issues with prostheses are not one-off issues, so your prosthetist will remain in your life indefinitely to help with any issues or concerns that occur. Emotional rehabilitation is seldom ever complete, so your therapist or counselor will also remain in your life to help you continue to cope with your new reality. Plus, emotional reactions can fluctuate from week to week — the bottom line is that you will never be alone.
Get Comprehensive Amputation Rehabilitation at Post Acute Medical
Support begins and ends with your rehabilitation team, and at Post Acute Medical, we are dedicated to assisting in your rehabilitation with a cohesive amputation rehabilitation plan, which includes an individualized treatment plan, work/home analyses and family counseling.
We know the importance of ongoing support, which is why our program also offers post-discharge services for you and your family.
If you are looking for experienced, professional clinicians to join your ongoing support rehabilitation team, find a Post Acute Medical location near you and schedule a tour of the facility.
Source: PostAcuteMedical.com
All content herein is owned by author exclusively. Expressed opinions are NOT necessarily the views of VNR, authors, affiliates, advertisers, sponsors, partners, technicians, or VT Network. Some content may be satirical in nature.
All images within are full responsibility of the author and NOT VNR.
Read Full Policy Notice - Comment Policy
































